Weight-Loss Jabs Linked to Hundreds of Life-Threatening Illness Cases
In an era that increasingly emphasizes body image and health optimization, the pursuit of effective weight-loss solutions has led many individuals to explore various options, including weight-loss injections. While some prefer the comfort of surgical interventions, others have turned to revolutionary injections that promise quick results without the need for rigorous diets or intense workouts. However, recent reports have unveiled a troubling connection between these weight-loss jabs and severe health complications, raising critical concerns about their safety and efficacy.
Understanding Weight-Loss Injections
Weight-loss injections, such as Semaglutide, Liraglutide, Mounjaro, Ozempic, and Wegovy, have gained traction in both medical and wellness circles, primarily marketed for their ability to suppress appetite and enhance metabolic rates. Designed for individuals struggling with obesity or weight-related health issues, these medications act by mimicking the effects of hormones that regulate appetite/hunger and food intake.
Mechanisms of Action
The action of these weight-loss jabs typically involves:
- Appetite Suppression: These injections send signals to the brain to decrease hunger, making it easier to consume fewer calories.
- Blood Sugar Control: By influencing insulin levels, they help in stabilising blood sugar, which can prevent cravings.
- Increased Energy Expenditure: Certain medications may stimulate metabolic processes, leading to increased overall energy expenditure.
Emerging Health Risks
While the initial benefits of weight-loss injections can be appealing, a growing body of evidence has demonstrated a concerning trend: these treatments are associated with various life-threatening illnesses, raising alarms among healthcare providers.
Reported Illnesses
Recent findings indicate that patients using weight-loss jabs have encountered a myriad of complications. These include:
- Gastrointestinal Problems: Issues such as nausea, vomiting, and diarrhoea have been frequently reported.
- Pancreatitis: Inflammation of the pancreas, characterised by severe abdominal pain, has surged among users.
- Kidney Complications: Acute kidney injury is a serious risk associated with dehydration from gastrointestinal side effects.
- Thyroid Tumours: Although rare, some studies have linked these injections to an increased risk of thyroid cancer.
- Cardiovascular Events: There are concerns regarding potential heart attack and stroke risks associated with certain formulations.
Statistical Insights
The statistics provide a sobering reflection of the potential dangers:
- According to a recent safety assessment, approximately 12% of users experienced significant side effects.
- The report highlighted that instances of acute pancreatitis rose by over 40% in patients receiving these injections compared to those who did not.
- Additionally, the risk of developing thyroid issues increased by nearly 30% among long-term users.
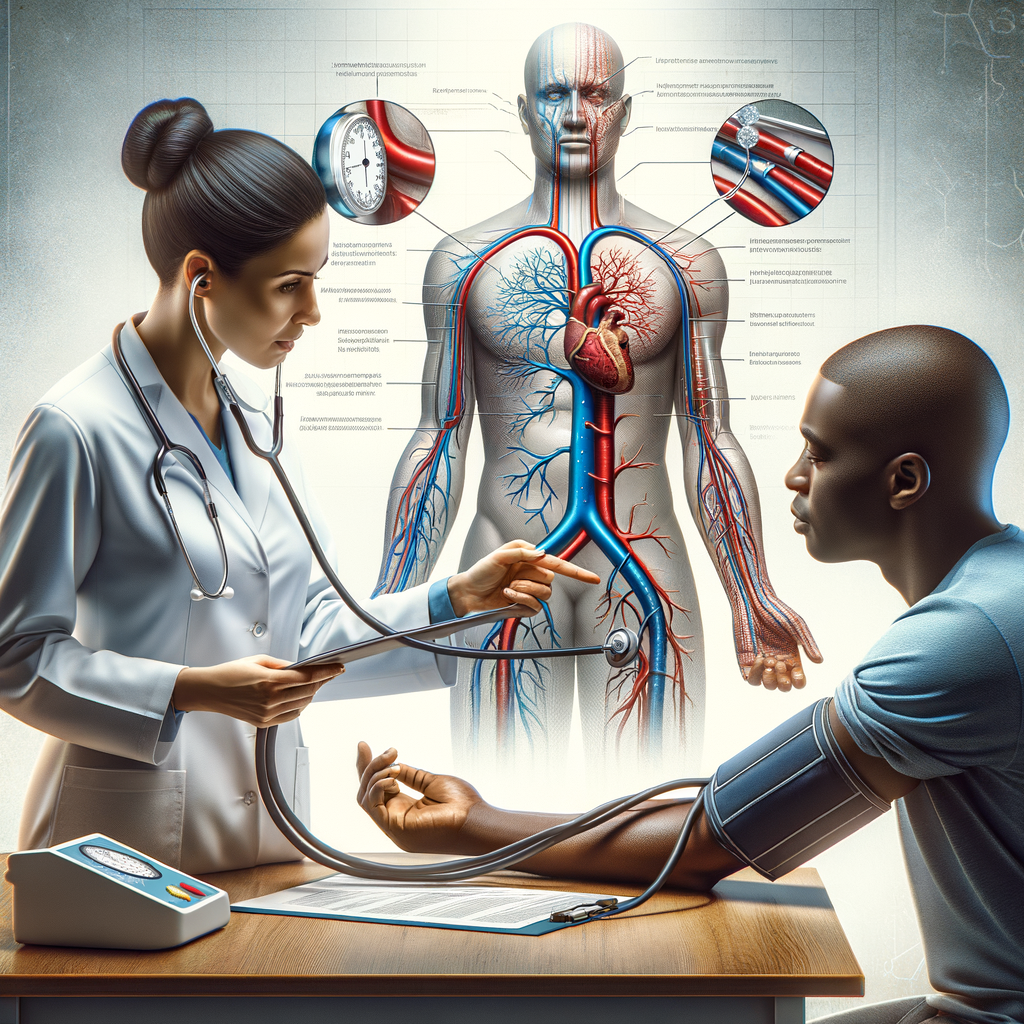
The Importance of Medical Supervision
With emerging evidence linking weight-loss jabs to severe health risks, the importance of medical supervision cannot be overstated. Patients contemplating this treatment option should:
- Consult with a healthcare professional to evaluate individual health risks.
- Discuss potential benefits versus risks before commencing treatment.
- Engage in regular monitoring of health indicators throughout the treatment process.
Conclusion
While weight-loss injections offer a promising avenue for many seeking to shed excess weight, the associated health risks cannot be ignored. The surge in reports linking these jabs to hundreds of life-threatening illness cases compels both patients and healthcare providers to prioritize caution and thorough medical oversight. As the landscape of weight-loss solutions continues to evolve, informed decisions grounded in comprehensive health assessments must remain at the forefront of any weight-loss journey.
There you have it… See what works for you…
Campbell M Gold
To Create Health, Wealth, Success, and Longevity through the Power of Your Subconscious Mind, Visit: Campbell M Gold.com
Visit The Store and see what else can be of help